The COVID-19 pandemic has wreaked havoc globally, challenging leaders and healthcare professionals at every turn. Recently, on April 10th, the H.J. Res 7 bill was signed into law, calling for the end of the national emergency declaration for COVID-19, which was put in place to mitigate the pandemic’s effects. This triggers the process and timeline to phase out extensions that were allowed as part of the pandemic. As an employer, it is important to understand what this means for your organization, particularly in terms of consumer-direct benefits and COBRA.
What is H.J. Res 7?
H.J. Res 7 stands for House Joint Resolution 7. It is a bipartisan resolution passed by the U.S. House of Representatives calling for the end of the national emergency related to COVID-19. This would terminate certain provisions of the Coronavirus Aid, Relief, and Economic Security (CARES) Act and the Families First Coronavirus Response Act.
Additional extensions were permitted for:
- Time a participant has to elect coverage
- Time a participant has to pay for COBRA
- Dispute denials of claims
- Amount of time to submit claims for coverage
- Special health plan enrollment period extensions
- Time a participant has to notify a health plan of a qualifying event or disability
Timeline Considerations for COBRA Continuation Services
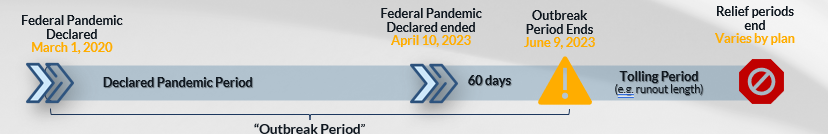
The guidance disregards election, payment and submission requirement timeframes for the Outbreak Period. The “Outbreak Period” acts as a pause on typical deadlines that apply for COBRA and other benefit plans, including the time a participant must elect COBRA and the time a participant must pay for COBRA coverage.
The “Outbreak Period” will end 60 days after the National Emergency ends. The National Emergency was terminated effective April 10, 2023, placing the Outbreak Period’s end as June 9, 2023. In March 2021, guidance indicated that individual extensions could not exceed 12 months.
COBRA deadlines are based on the individual’s qualifying event date. Because the Outbreak Period is disregarded when applying COBRA election and payment deadlines, a qualified beneficiary has the lesser of 1 year or+ 60 days after the end of the Outbreak period to elect and 45 days after that to pay the initial premium.
Timeline Considerations for Consumer-Directed Benefit Plans
Participants with a runout period that expired on or after March 1, 2020, received an extended period of time to submit claim reimbursements for eligible expenses from their Flexible Spending Accounts (FSA).
Runout periods were not to exceed 12 months beyond the end of the runout period for the plan year. Taking into consideration the 12 months and the official Pandemic period ending as of April 10, 2023. For example, if the plan year ends on 12/31/22 with a 90-day runout, then on June 9, 2023 the outbreak period ends, and the runout clock begins. The last day to submit claims would be September 7, 2023.
Future-proofing Health Care Policies
As the world transitions to post-pandemic healthcare, it’s as important as ever for employers to keep their healthcare policies and benefits future-proof. Given the uncertainty surrounding the COVID-19 pandemic, many organizations found themselves with outdated policies and were unable to react in real time. However, they can learn from this period to implement policies that can adapt to future threats.
Employers that focus on the health and well-being of their employees have a crucial role to play in the post-pandemic healthcare landscape. Similarly, they can align their health benefits policies to reflect the reduced risk associated with COVID-19. Employers can take advantage of this period to innovate and change their healthcare policies to suit the changing healthcare landscape. For instance, offering discounted gym memberships, healthy meal options, and exercise incentives could help employees boost their immune systems and reduce the chance of contracting the virus.
Moving Forward
The H.J. Res 7 bill signifies the end of an era in the battle against COVID-19. However, with the changing healthcare landscape, organizations must adapt to ensure they keep their employees’ health and well-being at the forefront. By innovating and making policy changes that align with changing consumer behavior, organizations can position themselves for success in the post-COVID-19 era. The end of the pandemic may signal a new beginning, but for employers, it’s an opportunity to reassess and enhance healthcare policies to future-proof their organizations.
IRS Guidance on COVID-19 Related Services Considered Preventive Care
Updated on June 28, 2023: The IRS has recently issued an advanced version of Notice 2023-37 to revise previous guidance in response to the conclusion of the coronavirus (COVID-19) public and national health emergencies.
During the COVID-19 pandemic, the Treasury Department and IRS issued Notice 2020-15, which allowed HDHPs to provide medical care services and items related to COVID-19 testing and treatment before the minimum deductible was met, without affecting HSA eligibility.
Following the end of the COVID-19 National Emergency and Public Health Emergency in spring 2023, the IRS has determined that the relief provided for these COVID-19 services for HDHPs will end for plan years ending on or before December 31, 2024. After this date, plans will no longer be able to offer benefits for COVID-19 testing and treatment without applying the deductible.
Under current guidance, COVID-19 testing and treatment benefits are not considered “preventive care” for pre-deductible coverage. However, if the United States Preventive Services Task Force (USPSTF) were to recommend COVID-19 testing with an “A” or “B” rating in the future, the services would be treated as “preventive care” and would be eligible for pre-deductible coverage under a qualified high deductible health plan.
Interested in learning more? Sign up for our webinar, “Benefits in Turbulent Times: Impact of the End of the Pandemic“



